A Curious Cure
Anticholinergic Smoking Cessation Therapy
Nov 2008
Citation: Lux. "A Curious Cure: Anticholinergic Smoking Cessation Therapy." Erowid Extracts. Nov 2008;15:8-11.

|
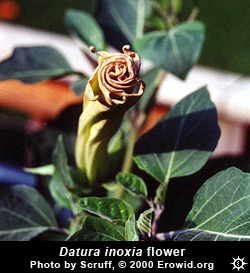
Tropane Alkaloids
A number of plants in the Solanaceae family (Datura spp., Brugmansia spp., Atropa spp., and Duboisia spp.) contain the tropane alkaloids hyoscyamine, atropine, and scopolamine, which induce delirium and hallucinations in sufficient doses. Growing wild in many parts of the world, with some cultivated for their striking blooms, they are notorious for causing intense intoxication and for their use by young, naïve seekers.Erowid has published hundreds of first-time experience reports with solanaceous plants, although few take them a second time. Media sources regularly report on incidents where people who have ingested them end up hospitalized. While powerfully psychoactive, their effects are widely experienced as too unpleasant (or considered too dangerous) to give them much of a following.
Nonetheless, tropane alkaloids have been valuable as entheogens and medicines for thousands of years. Smoking cessation therapy is one of their newer applications. Currently, several clinics in the United States offer smoking cessation treatments employing scopolamine injections, some of which also include atropine and/or an antihistamine, followed up by additional scopolamine in tablets or patches.
Pharmacology and Effects
Scopolamine and atropine are similar to one another in action and effects, though scopolamine is 7-8 times more potent.1 Both are anticholinergics that blockade acetylcholine receptors in the brain, and prevent neurotransmitters (the brain's chemical messengers) from binding at those sites.2 They bind to the muscarinic receptors, but show little activity at the nicotinic receptors, the other acetylcholine-based receptor type.2Depending on dose, scopolamine and atropine can produce delirium lasting anywhere from 3 to 24 hours or more, during which vivid hallucinations are common. Unlike the visuals experienced with serotonin-affecting psychedelics like LSD and mescaline, tropane alkaloid hallucinations often seem so substantial that they cannot be distinguished from reality. Physical symptoms include dry mouth, blurred vision, and dizziness.
|
History and Medicine
Theophrastus, a student of Aristotle, wrote about the hallucinogenic effects of datura in the fourth century BCE.3 The plant also appears frequently in Hindu and Buddhist religious art and literature,4 and has likely been used in Indian ethnomedicine for centuries.
The Persian physician Avicenna (980-1037 BCE) described Datura metel as a narcotic medicine.5 Datura inoxia has been consumed as an entheogen by Native Americans in the southwest United States since at least 1200-1250 CE.5 The Aztecs, who referred to D. inoxia as toloache, used it as a fever remedy.5 Brugmansia is employed in South America as an entheogen, and some species are included as admixtures in ayahuasca.6In addition to producing visionary effects, scopolamine and atropine are approved by the FDA for diverse medical uses. Atropine was introduced to western medicine in the early nineteenth century by British soldiers who learned of its use in treating respiratory disorders in India.7 It has since been used as an asthma treatment, along with scopolamine and various other anticholinergics.7 Atropine is considered an "essential medicine" by the World Health Organization for its use as a pre-operative sedative, a poison antidote, and in ophthalmologic procedures.8,9 Scopolamine is available in transdermal patches to treat severe motion sickness, nausea, and dizziness.
Anticholinergics and Smoking Cessation
The use of scopolamine and atropine for smoking cessation has not been approved by the FDA. However, as both compounds have been approved for other conditions, they may be prescribed "off label" for this use.In the 1950s, atropine was found to counteract some of the deadly effects of anticholinesterase nerve agents such as sarin gas by blocking the muscarinic receptors.1 Using a similar logic, Glick et al. noted in 1970 that scopolamine may inhibit nicotine's addictive effects by blocking its site of action.10 Scopolamine, atropine, and nicotine all affect acetylcholine receptors. Scopolamine and atropine primarily block the muscarinic receptor subtypes while nicotine acts primarily on the nicotinic receptor subtypes.
An exploratory animal study found dose-dependent decreases in the self-administration of tobacco smoke in two rhesus monkeys that had been administered scopolamine; however, scopolamine's effect of increasing thirst may have contributed to the decrease in smoking.10
IIn 1986 a pilot study examined anticholinergic therapy in 500 human patients for a twelve-month period.11 Dr. Kirk Voelker, an advocate of the therapy, explains the theory for nicotine withdrawal that informed the pilot study:
An exploratory animal study found dose-dependent decreases in the self-administration of tobacco smoke in two rhesus monkeys that had been administered scopolamine...
Bachynsky's [1986] paper [ ] suggested that there was competitive inhibition between nicotine and acetylcholine for the nicotinic receptors. [Chronic nicotine use thus leads] to an increase in acetylcholine stores in the brain. When the patient quit smoking, this excess of acetylcholine in the brain caused some of the physical effects of withdrawal. Bachynsky suggested that it took about 7-10 days for these acetylcholine stores to get back to normal. Thus the "hump" of physical withdrawal was in the first 7-10 days.12In Bachynsky's theory, using anticholinergics to block the muscarinic receptors should shield them from excess acetylcholine, and thereby prevent physical withdrawal. In the pilot study, during their out-patient visits, patients were initially given intramuscular injections of 0.2 mg atropine and 0.2 mg scopolamine. Five minutes later they were given two subcutaneous injections totaling an additional 0.2 mg atropine and 0.2 mg scopolamine, plus 10 mg of the antipsychotic chlorpromazine.11 For the 13 days following their injections, patients received oral and/or transdermal anticholinergics.11 86.8% of patients were smoking-abstinent at two months, and 39.8% remained non-smoking at one year--higher than expected success rates for smokers using "the average smoking cessation program", Bachynsky claimed.11
This study was completed prior to the widespread use of bupropion (Zyban) and varenicline (Chantix) for smoking cessation. Research into the effectiveness of newer pharmacotherapies at 13 months shows the rate of continuous abstinence was 10.3% for placebo, 14.6% for bupropion, and 23% for varenicline.13 Depending on the form (transdermal patch, inhaler, gum, sublingual tablet, intranasal spray), nicotine replacement therapy abstinence rates range from 14 to 24% after one year.14 These figures are consistent with Bachynsky's claim.
Glick et al. 1970 and Bachynsky 1986 are the primary peer-reviewed studies supporting anticholinergic smoking cessation therapy.15 However, the authors of the 1970 monkey study caution that their results may not be generalizable to humans, and the 1986 pilot study has methodological problems, such as failing to use a comparison/control group. It should also be noted that about three years after the 1986 paper was published, its author was sentenced to just over ten years in jail for insurance fraud,16 and his medical license was revoked.
Two additional smoking cessation studies have reported results similar to Bachynsky. One followed 45 subjects and found a one-month success rate of 76%.17 The researcher holds a patent on the technique18 and is a primary shareholder in a clinic that administers the therapy. Another provider, the Welplex Stop Smoking Clinics, conducted a study of 200 patients with either a 78% or 88% smoking cessation success rate at 60 days (there is a discrepancy in the numbers provided in their report), and a 56% success rate at one year.19 Such results are encouraging, but reports lacking peer review that have been conducted by those with a direct financial stake in the success of a treatment should be viewed with caution.
Although the procedure appears to be relatively safe, delirium is sometimes a problem. In one case, a 59-year-old man who received anticholinergic smoking cessation therapy suffered delusions of persecution by his family. He was hospitalized after contemplating suicide and the murder of his wife.15 After discontinuing the oral anticholinergic regimen, his symptoms disappeared within 48 hours.
The Treatment Experience
The initial injections of scopolamine and atropine produce psychoactive effects such that patients are instructed not to drive. Forgetfulness, euphoria, intoxication, and hallucination are reportedly common. However, those effects usually subside within the first 12 hours. While the two weeks of follow-up medication may be sufficient to push some patients off baseline, it does not generally produce the kind of delirium associated with acute solanaceous plant intoxication.Nicotine's physical withdrawal symptoms include depressed mood, irritability, nicotine craving, and anxiety.20 The two people we talked with who had undergone this treatment and the doctor who worked at a clinic offering the procedure all agree that it effectively eliminates physical withdrawal symptoms. Since the acute psychoactive effects of the treatment subside after 12 hours, it is clear that relief from withdrawal symptoms is not simply due to the effects being masked by a mental fog, though the pharmacological mechanism behind this relief is still a matter of speculation.
Mind or Matter?
It is possible that the psychological effects brought on by the initial psychoactive dose of scopolamine and atropine contribute to the quitting process. Such experiences are not unknown; the modern use of ibogaine to treat opiate dependence involves physiological and psychological elements that can be difficult to disentangle.21,22 In a related example, Leo Zeff reported losing all desire for cigarettes after a psychedelic therapy session in which he addressed his smoking.23A doctor who worked in a clinic offering anticholinergic therapy for smoking agreed:
How can we ever fully differentiate between pharmacologic and psychodynamic intervention? I believe both aspects were strong determinants of successful outcome. I would take advantage of this mythos of the strong and powerful medication, telling patients that we know these medications well and use them safely; that they do make you feel funny, and that is the therapy working; that even before they were pharmacy medicines, the plant sources were healing medicines for native peoples.24Whether the primary cause is physiological or psychological, this doctor is convinced that scopolamine treatment can be effective in helping smokers quit.
Some patients came in through ads, but most came in because they knew someone who successfully stopped smoking at the clinic. You take a 60-year-old southern gentleman with a 90-pack-a-year history (who tried to quit every way he could and always failed) who suddenly stops smoking after one two-hour visit without much difficulty; that is pretty damn impressive. It is enough to make one almost evangelical.24In the accounts that accompany this article, an anticholinergic smoking cessation program appears to have been effective in eliminating nicotine withdrawal symptoms. Yet, like many smoking cessation therapies, it does not curtail the long-term, ingrained behavior patterns and stresses that can lead people back to smoking months or years after treatment. Nevertheless, these powerful deliriants may constitute a useful approach for some patients who need help getting started with the quitting process.
|
No Craving Whatsoever#
by Scruff | |
| I decided to get serious again about quitting smoking, after a 27-year, pack-a-day cigarette habit, when I learned I had Chronic Obstructive Pulmonary Disease. I've been part of the Erowid crew for a long time; in the first two years that the Experience Vaults were online, I was the second most active report reviewer, after Fire. I had a particular interest in reviewing datura reports, and have grown datura plants in my garden for a long time. My doctor had previously mentioned a clinic that featured a "stop smoking shot", so I visited their website. When I read that scopolamine was a constituent of the injection, I was more excited than I'd ever been to quit smoking. I mean, really, I thought... a controlled datura alkaloid experiment? Sign my silly ass up! When I made an appointment, they asked me to arrange for someone to pick me up from the clinic. They made me wait nearly two hours, during which I smoked at least eight cigarettes... it was kind of creepy, with everyone who was waiting for treatment smoking like fish. It was fun to watch the different people ahead of me as they left the clinic after their shot. During the session, a doctor gave me three injections--one IM and two subcutaneous under each ear. I could hear the fluid going under my skin during the injection. The principle drugs in the cocktail are scopolamine and atropine, although other drugs are sometimes included as part of the initial injection, depending on the needs of the person seeking treatment.
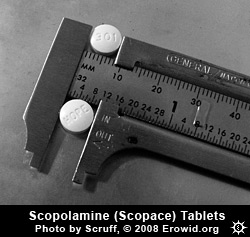
I got the shots around 1:00 pm and regained minimal self-motivated functioning at about 7:00 pm, but the effects were strong until morning. After the initial shot in the doctor's office, the treatment required that I take 0.2 mg of scopolamine (Scopace) twice a day, orally. I was prescribed two doses each day but I'd guess on the average I took 3-5 doses a day, because I enjoyed the effects. I was supposed to do the follow-up therapy for 7-10 days; I did three weeks, with the Algonquin coming-of-age ritual in mind. That was enough to get some psychoactive effects at night, but not especially pronounced. I had dry mouth and dilated pupils during the day, and usually felt very other-worldly and detached. I was easily distracted and unable to return to the present task, which is unusual for me. I was successful in quitting for twenty months. I'm smoking again now, but much less than ever before. The best I'd done previously was three months and every day was a torment. It was actually quite remarkable at first--no craving whatsoever, unlike any other method I'd tried, including a disastrously unpleasant reaction to Zyban that didn't reduce my cravings at all. Thinking about the fact that cigarettes are available nearly anywhere I go didn't trigger the "I need one NOW" response, the way it did with other methods of quitting. |
Three Tries and Still Working on Quitting#
by Wonderama |
| I heard about scopolamine/atropine therapy from Scruff. After the first time I tried it, all was well for five weeks or so, then I started to get depressed. I'm prone to depression to begin with, and smoking cessation triggers it. I wasn't on antidepressants at the time, and I was pushing suicidal, so I started smoking again; the depression lifted within a couple of days. The second time was about a year later, and that failure seemed to boil down to bad timing. My stepfather passed away three weeks after I was treated, so I picked it back up. I was, however, prepared for the depression, and had gone back on antidepressants (150 mg Effexor daily) a couple of months before I was treated. The most recent time, I was, again, prepared with the meds. What I've found, and what I think would have ultimately caused me to fail with the prior treatments (if other stuff hadn't precipitated my failure), is that the treatment obliterates all physical withdrawal, but doesn't set one up well for breaking the habit and dealing with the psychological stuff that needs attention. As far as any psychoactive effects, I mostly had euphoria, along with very blurry vision and memory loss while on the scopolamine. Once the medicine runs out, the psychological stuff hits me hard. I was interested in the treatment at first because it took away the most challenging part of the withdrawal, and I did it again because I really thought that's where I'd have the most problem. I'm still working on quitting. After a lot of thought, I've decided that the nicotine patch is what works best for me. My most successful quit was for nearly a year, via nicotine replacement therapy; I was still getting nicotine for a good long time, which gave me one less thing to stress about and allowed me to focus on dealing with the other stuff, which is clearly where things fall apart for me. |
References #
- Ketchum JS. Chemical Warfare: Secrets Almost Forgotten. ChemBooks Inc. 2006.
- Nestler EJ, Hyman SE, Malenka RC. Molecular Neuropharmacology: A Foundation for Clinical Neuroscience. McGraw-Hill. 2001.
- Theophrastus. Historia Plantarum. c. 201 BCE.
- Parker RC, Lux. "Psychoactive Plants in Tantric Buddhism". Erowid Extracts. Jun 2008;14:6–11.
- Rätsch C. The Encyclopedia of Psychoactive Plants. Park Street Press. 1998. 203,196.
- Keeper of the Trout. Ayahuasca: alkaloids, plants & analogs, Sec 3: Part 3: Purported traditional ayahuasca admixtures. Erowid.org/books_online/ayahuasca_apa.
- Rodrigo GJ, Rodrigo C. "The Role of Anticholinergics in Acute Asthma Treatment; An Evidence-Based Evaluation". Chest. 2002;121:1977–1987.
- World Health Organization. Essential Medicines, 15th Ed. Mar 2007. Accessed Oct 4, 2008; www.who.int/medicines/publications/EML15.pdf.
- Sowka, JW, Kabat, AG. "Open Your Eyes to Cycloplegia". Review of Optometry Online. Mar 15, 2007;144:3.
- Glick SD, Jarvik ME, Nakamura RK. "Inhibition by drugs of smoking behaviour in monkeys". Nature. Aug 1970;227(5261):969–71.
- Bachynsky N. "The Use of Anticholinergic Drugs for Smoking Cessation: A Pilot Study". Int J Addict. 1986;21(7):789–805.
- Voelker KG. "Information for Physicians: An Interview with Kirk G. Voelker, MD, FCCP". QuitDoc Smoking Treatment Network. 2007. Accessed Oct 3, 2008; www.quitdoc.com/doctor/interview_voelker.html.
- Jorenby DE, Hays JT, Rigotti NA et al. "Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial". JAMA. Jul 2006;296(1):56–63.
- Silagy C, Lancaster T, Stead L, et al. "Nicotine replacement therapy for smoking cessation". Cochrane Database Syst Rev. 2004:CD000146.
- Clarke LA, Cassidy CW, Catalano G, Catalano MC, Carroll KM. "Psychosis Induced by Smoking Cessation Clinic Administered Anticholinergic Overload". Ann Clin Psychiatr. 2004;16:171–5.
- United States of America v. Nicholas Bachynsky, 924 F.2d 561 (5th. Cir. 1991).
- Voelker KG. "Efficacy of a County Government Employee Benefits Smoking Cessation Program Utilizing an Anticholinergic Intramuscular Injection Combined with Counseling". Conference poster description. Chest (supplement) Oct 2005;128(4):387S.
- Voelker KG. Method of decreasing nicotine withdrawal symptoms during smoking cessation. USPTO Application #: 20050226920. Oct 13, 2005.
- Welplex. "Retrospective Study for Anticholinergic Blockade in Smoking Cessation". Accessed Sep 30, 2008; www.stopsmokingcharlotte.com/Retrospective Study One.pdf.
- Spinella M. The Psychopharmacology of Herbal Medicine: Plant Drugs that Alter Mind, Brain, and Behavior. MIT Press. 2001. 101.
- Dobkin de Rios M, Grob CS, Baker JR. "Hallucinogens and Redemption". J Psychoactive Drugs. 2002;34(3):239–48.
- Karpetas S. "Ibogaine as Therapy: Sandra Karpetas Speaks" (interviewed by J Hanna). The Entheogen Review. 2004;13(1):1–11.
- Stolaroff MJ. The Secret Chief Revealed. MAPS. 2004.
- Holidoc. Personal communication. 2008.